A Holiday Cheers
 The holidays are officially upon us and so is your growing baby bump!
The holidays are officially upon us and so is your growing baby bump!
Pregnancy can be challenging, especially with the commotion of the holiday season. In addition to the normal complexities of growing another human in your belly, many people work longer prior to the holiday season, and have additional financial and emotional stressors during this time. Are you wondering how you will keep your spirits up and your stress down this time of the year?
From Cocktail to Mocktail, Keeping Your Spirits Up Without Spirits
‘Tis the season for family, celebrating old traditions and starting new ones, and giving as much as we can. With all the stress, many enjoy ending the day with a refreshing drink. When you're pregnant, though, you will need to be a little more careful what you fill your glass with. Consuming alcohol is generally a no-no during pregnancy, since there is no known safe amount of alcohol use during pregnancy. The good news is that there are many great holiday mocktails for pregnant women that taste just as good as their alcoholic counterparts, and take little-to-no-time to throw together. So this holiday season drink your eggnog without the rum (and use a pasteurized kind), swap your bubbles for non-alcoholic fizz, warm up with mulled apple juice in place of a traditional spiced wine or cider, and brush up on seasonal mocktails.
Common Skin Conditions While Pregnant
 During pregnancy, your body will go through a multitude of changes. While many of those changes are internal, some are more prevalent physically, including skin conditions that may arise. There are many common skin conditions that can occur during pregnancy and most of them disappear postpartum. Most common skin conditions can be broken down into three categories: hormone-related, preexisting, and pregnancy-specific.
During pregnancy, your body will go through a multitude of changes. While many of those changes are internal, some are more prevalent physically, including skin conditions that may arise. There are many common skin conditions that can occur during pregnancy and most of them disappear postpartum. Most common skin conditions can be broken down into three categories: hormone-related, preexisting, and pregnancy-specific.
Hormone-Related Skin Conditions
Many skin conditions that women will experience during pregnancy are due to hormonal changes that the body goes through. Pregnant women experience sudden and dramatic increases in estrogen and progesterone, in addition to a number of other hormones. Some of the most common hormone-related skin conditions include hyperpigmentation, stretch marks (or striae gravidarum), vascular changes, and changes to your hair and nails.
Hyperpigmentation
Dark patches or spots that appear on the skin are known as hyperpigmentation. Hyperpigmentation is caused by an increase in naturally occurring melanin. Regularly, hyperpigmentation will resolve itself after delivery, but in some cases, it may take several years until it disappears completely. Melasma or “pregnancy mask” is an example of hyperpigmentation that appears as brown spots on different features of the face. Limiting sun exposure during pregnancy can help reduce melasma symptoms.
What is a Non-Invasive Prenatal Test?

A Non-Invasive Prenatal Test (NIPT, for short) can also sometimes be called a Non-Invasive Prenatal Screening (NIPS). This is a method used to determine the risk of a fetus being born with certain genetic abnormalities.
How Does a NIPT or NIPS Work?
This testing method analyzes small fragments of DNA that are circulating in the pregnant woman’s blood. During pregnancy, a mother’s blood contains a mixture of cell-free DNA (cfDNA) that comes from both her cells and the cells from the placenta. The placenta is tissue in the uterus that links the mother’s blood supply to the fetus. Cell-free DNA, is a certain type of DNA that is free-floating and not within a cell, unlike most DNA which is found inside a cell’s nucleus. Throughout a woman’s pregnancy, cell-free DNA is often shed into the mother’s bloodstream. These placental cells contain DNA usually identical to the fetus’ DNA. By analyzing this cell-free DNA from the placenta, expecting mothers are provided an opportunity to find early detection of certain genetic abnormalities.
How is the NIPT Administered?
A pregnant woman at 10 to 13 weeks, can get a Non-Invasive Prenatal Test by getting their blood drawn. This test poses no risk to the mother or their baby. The blood sample is then sent to a lab where technicians analyze the results and report the findings back to the ObGyn. Results can be expected within 8 to 14 days from when they are sent.
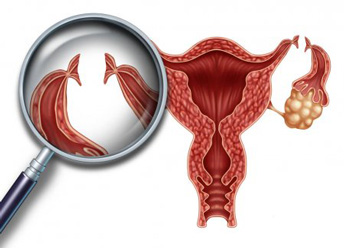
September is Ovarian Cancer Awareness Month: What You Should Know
 September is recognized as Ovarian Cancer Awareness Month. According to the American Cancer Society, ovarian cancer ranks fifth in cancer-related deaths among women, and the chance of a woman getting ovarian cancer in her lifetime is 1 in 78. Ovarian cancer mainly develops in older women with about half of those diagnosed age 63 or older. At any age, it’s important to know the facts about ovarian cancer.
September is recognized as Ovarian Cancer Awareness Month. According to the American Cancer Society, ovarian cancer ranks fifth in cancer-related deaths among women, and the chance of a woman getting ovarian cancer in her lifetime is 1 in 78. Ovarian cancer mainly develops in older women with about half of those diagnosed age 63 or older. At any age, it’s important to know the facts about ovarian cancer.
What Causes Ovarian Cancer?
Researchers have yet to find an exact cause of ovarian cancer. Recent findings about the cause indicate that it starts in the cells located at the tail end of the fallopian tubes and not the actual ovary. There are many theories about the cause of ovarian cancer. For instance, some researchers think that there may be some relationship between ovulation and the risk of developing ovarian cancer. This correlation is due to both pregnancy and taking birth control pills both lowering the risk of ovarian cancer.
What are Ovarian Cancer Risk Factors?
There are a few risk factors that are associated with ovarian cancer. However, it is important to note that having a risk factor, or a few risk factors, does not mean that you will get the disease. Risk factors are anything that increases your chance of getting a disease like cancer.
As mentioned before, half of the women diagnosed with ovarian cancer are age 63 or older. As you age, the risk of developing ovarian cancer increases. Ovarian cancer is very rare in women younger than 40 and most ovarian cancer cases develop after a woman goes through menopause. Cigarette smoking is a risk factor. Women who have had children over the age of 35, or have never had children at all, tend to have a higher risk of ovarian cancer as well. Endometriosis, polycystic ovarian syndrome, and infertility have all been identified as risk factors. Family history may also indicate an increase in ovarian cancer risk. Several ovarian cancer susceptibility genes have been identified.
January is Cervical Cancer Awareness Month
Cervical Cancer Awareness
 Cervical cancer was a common disease in women in the past, but routine Pap smear screening has reduced the incidence of cervical cancer dramatically. A well-woman visit is a great opportunity for a female patient and their Ob/Gyn provider to review her health, conduct screenings, and discuss preventive health care steps. Since January is Cervical Cancer Awareness Month, this article will discuss facts you should know about cervical cancer and the importance of screening and its protocols.
Cervical cancer was a common disease in women in the past, but routine Pap smear screening has reduced the incidence of cervical cancer dramatically. A well-woman visit is a great opportunity for a female patient and their Ob/Gyn provider to review her health, conduct screenings, and discuss preventive health care steps. Since January is Cervical Cancer Awareness Month, this article will discuss facts you should know about cervical cancer and the importance of screening and its protocols.
What is Cervical Cancer?
Cervical cancer occurs in the cells of the cervix, which is the lower part of the uterus that connects with vagina. Various strains of HPV (Human papillomavirus) which is a sexually transmitted infection (STI) play a role in causing most types of cervical cancer. It is commonly seen in women who smoke and those who engage in high-risk sexual activities. Other risk factors are multiple sexual partners, early sexual activity, a weak immune system, and having other STIs.
Following exposure to HPV, the immune system fights the virus. However, in a small percentage of females, this virus may survive for years, later converting the cervical cells into cancer cells. The symptoms of cervical cancer include vaginal bleeding following intercourse, intermenstrual bleeding, heavy vaginal discharge which may be bloody with a foul odor, pelvic pain, or pain during intercourse. HPV infection, however, has no symptoms.
The Benefits to Cord Blood Banking
 July is Cord Blood Awareness Month. There are often many questions when it comes to cord blood, its benefits, and why people choose to donate or store it. In this article you can learn more about cord blood and help make an informed decision on what to do with your own cord blood after birth.
July is Cord Blood Awareness Month. There are often many questions when it comes to cord blood, its benefits, and why people choose to donate or store it. In this article you can learn more about cord blood and help make an informed decision on what to do with your own cord blood after birth.
What is Cord Blood Banking?
Before deciding if you want to bank cord blood, it’s important to know what it is. Cord blood is the remaining blood from the baby that’s left in the umbilical cord and placenta after birth. Cord blood is unique in that it has a high concentration of stem cells. Stem cells have the ability to become mature blood cells including red blood cells, white blood, cells and platelets.
Cord Blood Uses
Cord blood and its use is at the discretion of you and your family. Usually for a yearly fee you can store your cord blood privately, to be used if and when it is needed by you or a family member. Private cord blood banking can be beneficial if you or a family member have an existing condition that can be treated using stem cells. Medically, it is unlikely that a child will develop a condition that can be treated with the child’s own stem cells.
Family Planning in a COVID-19 World
 You had baby names to consider, crunched the numbers financially and were already decorating the nursery in your head. 2020 was going to be your year to begin trying to get pregnant.
You had baby names to consider, crunched the numbers financially and were already decorating the nursery in your head. 2020 was going to be your year to begin trying to get pregnant.
And then COVID-19 struck.
Pondering the “best” time to get pregnant is a personal decision but as the global pandemic continues, couples are left wondering if this is really the safest time to get pregnant. Many have argued that a pandemic is no time to get pregnant. In fact, in May, a survey of 2000 women found that 34% wanted to delay pregnancy or have fewer children because of COVID-19. Others have argued that we will have a baby boom due to the pandemic and couples being stuck at home, potentially having more time and energy for intimacy.
While the decision to try to conceive may be more elusive due to COVID-19, this decision is absolutely personal, and there are no right or wrong answers. However, it is important to discuss your specific health history with your ob/gyn. Underlying health conditions, such as obesity, diabetes or heart disease, can increase your risk of pregnancy complications as well as the risk of poor outcomes with COVID-19. Fertility challenges also cannot be ignored and no one can guarantee that if you do choose to wait months, or years, for the pandemic to be over, that you will still be able to conceive. It is important to reflect on the urgency of your family planning. If you do decide that trying to conceive is the right choice for you - naturally or with fertility treatments - we have answered a few major pregnancy-related health questions to help guide your decision.
Would I Be High-Risk Because of My Pregnancy?
There is still a lot we don’t know about COVID-19 when it comes to pregnancy. As of now, there is no evidence that pregnant women are more likely to become seriously ill if they contract COVID-19. So far, COVID-19 infections don’t appear to cause congenital complications to the fetus. However, according to the Center for Disease Control and Prevention (CDC), pregnancy alone might increase your risk for severe illness.
Staying Cool in the Summer Heat While Pregnant
 While pregnancy in the summer can have its fair share of benefits, including fun, airy maxi dresses and delicious snacks of fresh fruit, the season can also cause its fair share of negatives. Pregnancy during summer can be an uncomfortable affair, as many pregnant women experience a spike in their body temperature during their pregnancy. Staying cool in the summer can be an important task to prepare for in advance.
While pregnancy in the summer can have its fair share of benefits, including fun, airy maxi dresses and delicious snacks of fresh fruit, the season can also cause its fair share of negatives. Pregnancy during summer can be an uncomfortable affair, as many pregnant women experience a spike in their body temperature during their pregnancy. Staying cool in the summer can be an important task to prepare for in advance.
Why Does a Woman’s Body Temperature Spike During Pregnancy?
While not every woman experiences a spike in body temperature during pregnancy, it is very common. Pregnant women have an increased amount of blood in their bodies that can cause them to feel warmer than they regularly might. In addition, hormonal changes and warmth generated by the baby can lead to an uncomfortable radiation of heat and hot flashes. While some of these symptoms are unavoidable there are many things you can do to stay cool during the toasty summer months.
Stay Hydrated
It should come as no surprise that staying hydrated is at the top of the list for staying cool during your pregnancy. Traveling with a reusable water bottle is an easy solution to make sure you’re drinking 8-12 cups of water a day. If you’re prone to forgetting, consider adding a reminder on your cell phone to stay on track. If you’re out in the hot sun, sweating will lead to dehydration much faster. Replenishing the electrolytes you lose while sweating is important in staying hydrated and avoiding any dizzy spells. Many foods can also help with hydration and electrolytes, including pickles, cucumbers, bananas and spinach.
Is Tubal Ligation Right For You?
 Tubal ligation (“tubes tied”) is a surgical procedure that many women elect to have done after they have decided they are done having children. It is categorized under permanent birth control, making the decision to have your tubes tied not a light or easy decision for many.
Tubal ligation (“tubes tied”) is a surgical procedure that many women elect to have done after they have decided they are done having children. It is categorized under permanent birth control, making the decision to have your tubes tied not a light or easy decision for many.
In the procedure, your fallopian tubes are either cut, tied or blocked to prevent pregnancy. This process prevents an egg from traveling from the ovaries to the uterus, where it could potentially be fertilized by sperm. Tubal ligation can be done anytime, including after childbirth and in combination with other abdominal surgeries, such as C-section. Once it has been performed, reversal/reversibility is quite difficult and, at times, impossible, requiring major surgery.
The Pros and Cons of Tubal Ligation
Many of the pluses and minuses of this permanent birth control are the same. For example, if you are done having children the permanence is a huge benefit over other birth control methods. However, if you still want to expand your family, that tubal ligation is permanant removes it as a birth control option. Unlike many other forms of birth control, tubal ligation is non-hormonal and once you recover from the low-risk surgery, there are very few risks. Additionally, this procedure may also decrease your risk of developing ovarian cancer, particularly if your fallopian tubes are removed, making it an attractive option to women at higher risk.
What do Pregnancy Cravings Mean?
 The stories about odd food cravings while you’re pregnant are true. While they may not be as humorous as movies and television shows make them out to be, cravings, as well as food aversions, are very common during pregnancy. In the U.S. alone, 50-90% of pregnant women experience cravings for specific foods, according to research. While there is no one specific cause tied to food cravings, researchers and doctors contribute the cravings to a few different factors.
The stories about odd food cravings while you’re pregnant are true. While they may not be as humorous as movies and television shows make them out to be, cravings, as well as food aversions, are very common during pregnancy. In the U.S. alone, 50-90% of pregnant women experience cravings for specific foods, according to research. While there is no one specific cause tied to food cravings, researchers and doctors contribute the cravings to a few different factors.
Why Does Pregnancy Cause Food Cravings?
Some of the most common theories as to why pregnancy causes food cravings include hormonal changes, sensory changes, a change of nutritional needs, and desires for comfort. Pregnancy is accompanied by a plethora of hormonal changes. Hormones can also affect a person’s senses, leading to new food experiences involving taste and smell. This leads to the second theory – sensory changes. Oftentimes, pregnant women will report that their sense of smell is stronger than before. A stronger sense of smell can work both ways for cravings. Stronger delightful smells can lead to cravings just as unpleasant, pungent smells can lead to food aversions.
VBAC: How To Predict Your Chance Of Success
 Cesarean sections can be a life-saving procedure for mother, baby or both. However, there are many reasons why vaginal birth is preferable when possible. More and more women are able to successfully give birth naturally after a cesarean (VBAC), however, there are many factors that go into calculating the odds of success.
Cesarean sections can be a life-saving procedure for mother, baby or both. However, there are many reasons why vaginal birth is preferable when possible. More and more women are able to successfully give birth naturally after a cesarean (VBAC), however, there are many factors that go into calculating the odds of success.
Benefits and Risks of Vaginal Birth After Cesarean
C-sections account for almost a third of all first births in the United States. The success rate of VBACs is between 60 to 80 percent. VBAC often carries fewer risks than a repeat cesarean and can offer a shorter recovery time and hospital stay, and a higher chance of successful breastfeeding. If you plan on having more children, being able to have a successful VBAC will also decrease your risks of placental problems associated with multiple c-sections.
However, a failed trial of labor that results in an emergency c-section is often riskier than a repeat planned c-section. Emergency c-sections carry a risk of uterine rupture, which can be life-threatening. The risk is low, occurring in about 1% of women attempting a vaginal birth after cesarean.